How to Use ASAM Guidelines to Get Authorization

What is ASAM?
ASAM (The American Society of Addiction Medicine) Criteria is the most common set of guidelines that payors and providers use to determine what level of care and length of treatment that the patient needs. They are typically referred to by the Utilization Review Specialist and case manager while they determine a treatment plan.
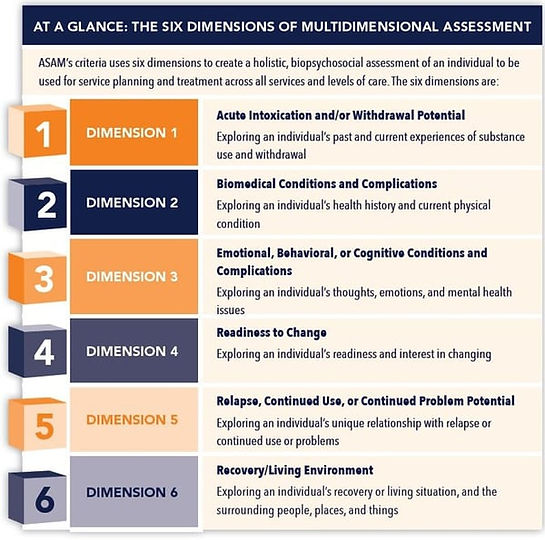
When your UR specialist calls for authorization, they will be asked to rate the patient’s condition on a 0-4 scale in the following six categories:
The insurer will then tally the score and use that number to determine the type of care the patient needs. This process will repeat during each concurrent review and until the patient discharges. Ats the client moves from Detox through IOP, the score will become lower.
ASAM guidelines provide a uniform way for payors, providers, and patients to communicate and coordinate care. Becoming familiar with ASAM guidelines and how they apply to the services you provide will assist in obtaining authorization and will also facilitate a successful, outcome-driven treatment plan for patients.
Contact Datapro’s Utilization Review Team for questions on ASAM guidelines or how to obtain the most days for your patient’s treatment.
For more information on this topic and much more, view our Behavioral Health Guide to Quick and Accurate Claims Processing. You can also download the PDF format by clicking on the image below.
CONTACT US
We help healthcare providers and facilities to optimize their finances and manage insurance billing so they can focus on high-quality care while maintaining confidence in their bottom line.
APPLY TO WORK TOGETHER
© aurora-hcs.com | All rights reserved | Created with Heart, Soul, & Strategy by Elise Cruz Company